Protective Bacterial Biofilm – What You Need to Know About Candida Auris Fungus
Candida auris is an emerging fungal pathogen responsible for causing severe infections in healthcare settings across the globe. First identified in 2009, it has proven to be a dangerous and multidrug-resistant species. The protective biofilm it forms plays a crucial role in its persistence and virulence. To better understand how to fight this ever-growing health threat, it’s essential to learn about its protective bacterial biofilm, common symptoms, and prevention methods.
Understanding the Protective Biofilm
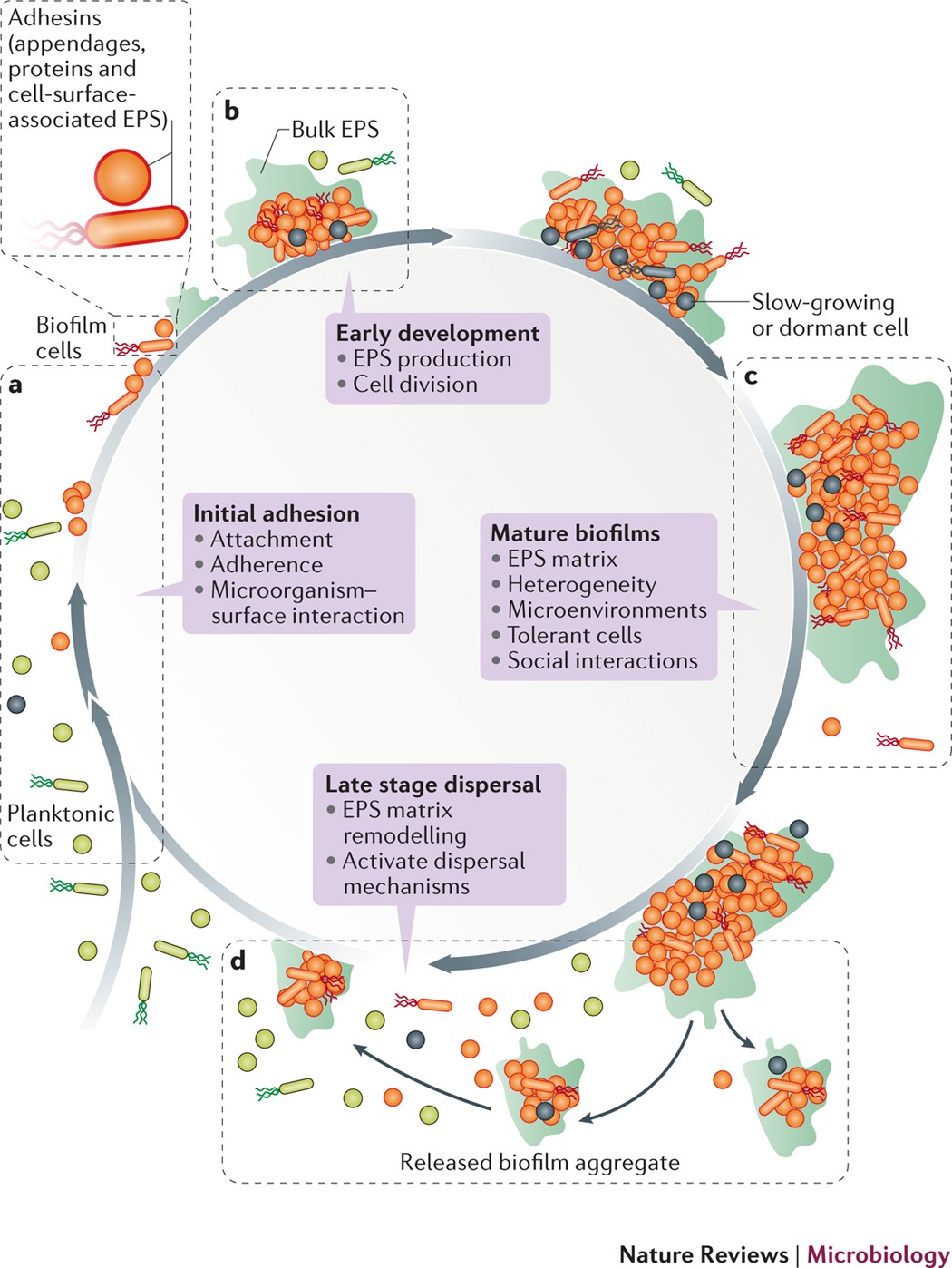
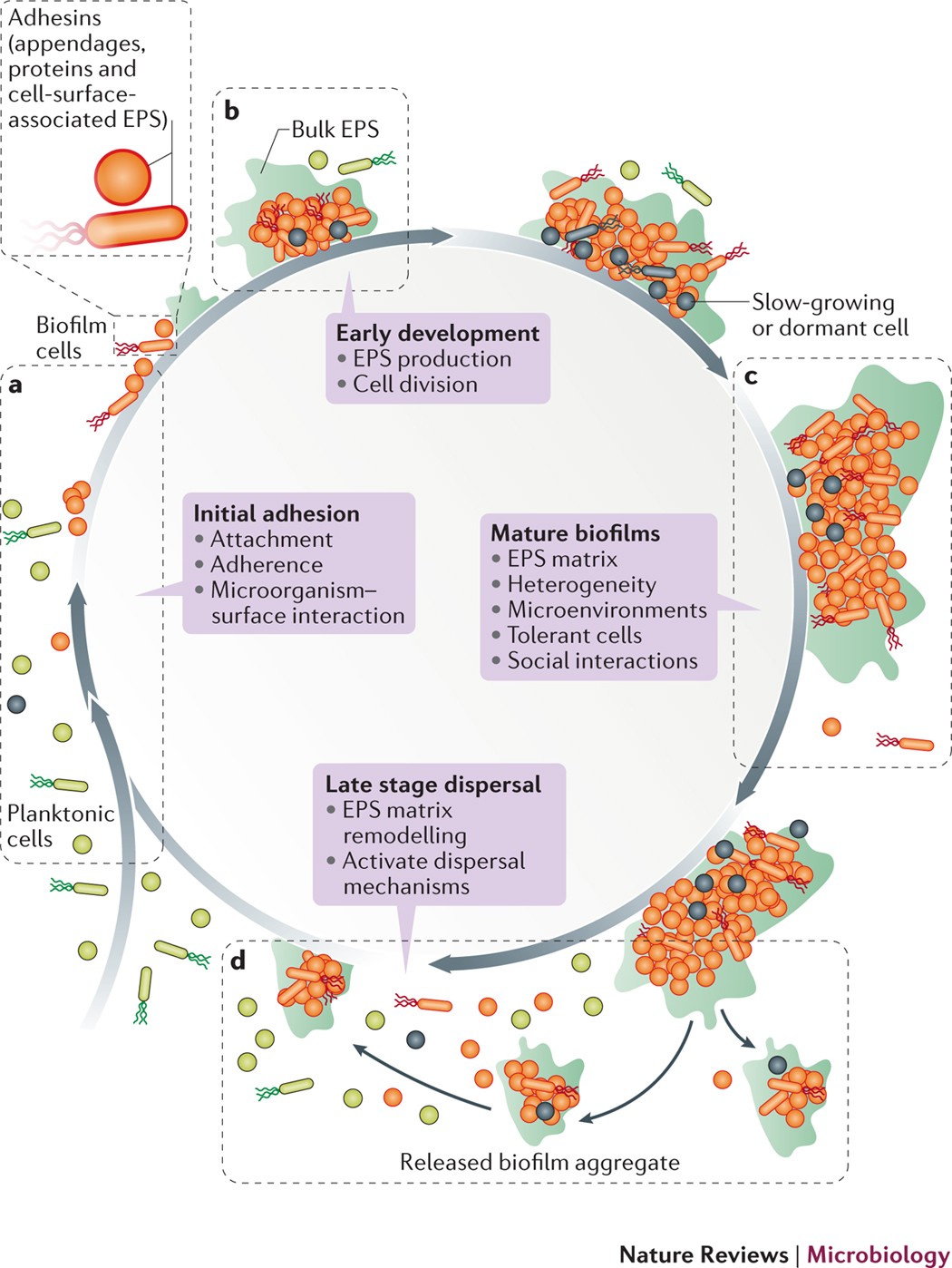
Biofilms are structured communities of microorganisms embedded in a self-produced matrix of extracellular polymeric substances (EPS). The EPS is composed of proteins, polysaccharides, and nucleic acids. In the case of Candida auris, the biofilm offers protection from the host’s immune response, enhances nutrient availability, and facilitates genetic transfer among the microbial cells. Sadly, it also contributes to increased resistance to antifungal drugs, making treatment more challenging.
Symptoms of Candida Auris Infection
Candida auris infection symptoms may vary, and it’s not uncommon for some infected individuals to be asymptomatic carriers. Here are a few possible symptoms that require medical attention:
1. Fever and chills unresponsive to antibiotics: These symptoms can indicate a systemic infection, and their persistence despite antibiotic treatment can indicate a fungal infection.
2. Wounds or areas of localized pain: This can signify localized infection within tissues or organs, leading to infiltrative growth of the fungal pathogen.
3. Respiratory symptoms: Unresolved respiratory symptoms can reveal a pulmonary infection caused by the fungus.
Dealing with Candida Auris Infection
Proper diagnosis of Candida auris is crucial for effective treatment. False identification can lead to inappropriate treatment, promoting drug resistance. Laboratory testing, such as matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry and molecular techniques, can aid in accurate diagnosis. Standard antifungal treatments, like fluconazole, are often ineffective due to high resistance rates. Therefore, alternative drugs such as echinocandins, amphotericin B, and newer antifungals are commonly used.
Prevention and Control Measures
Given the challenges in treating Candida auris infections, prevention is crucial. Implementing the following measures can help minimize the risk of infection:
1. Hand hygiene: Consistent use of alcohol-based hand sanitizers and practicing proper handwashing techniques can reduce transmission in healthcare settings.
2. Environmental cleaning: Thorough daily cleaning of high-touch surfaces with recommended disinfectants and cleaning agents is essential in the containment of the fungus.
3. Isolation precautions: Implementing contact precautions for patients diagnosed with or suspected of having Candida auris may reduce transmission among other patients in healthcare facilities.
In conclusion, the protective bacterial biofilm formed by Candida auris is a significant challenge to combat the multidrug-resistant fungal pathogen. Educating the public and healthcare professionals about proper hygiene, symptoms, and prevention measures can aid in reducing the spread of Candida auris infections and controlling this emerging threat. Ongoing research to develop novel treatment strategies targeting the biofilm is essential for successful infection management.